- After years of being criticised for not doing enough on tuberculosis, India got a pat on the back this week from the World Health Organisation for increasing the funding to fight the disease. The WHO’s Global Tuberculosis Report 2017 said India “stood out as a country in which the budget envelope for TB was substantially increased in 2017 (to US $ 525 million, almost double the level of 2016), following political commitment from the Prime Minister to the goal of ending TB by 2025”.
- All this money will come from domestic sources, making the commitment extra commendable. India has resolved to end TB by 2025, 10 years before the global deadline runs out in 2035. So how is India’s war on TB progressing?
Why is TB in India cause for global concern?
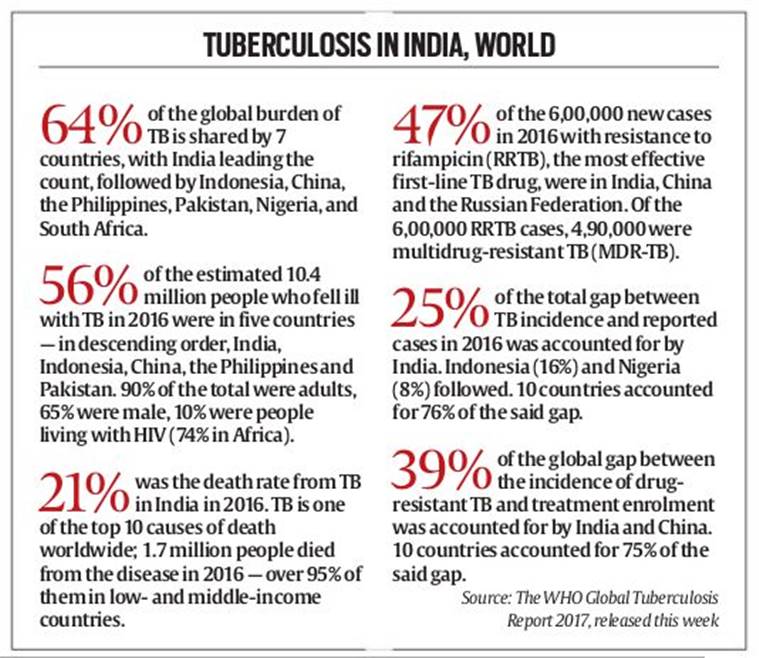
- According to the National Strategic Plan for Tuberculosis Elimination 2017-25, “TB kills an estimated 4,80,000 Indians every year, and more than 1,400 every day. India also has more than a million ‘missing’ cases every year that are not notified, and most remain either undiagnosed or unaccountably and inadequately diagnosed, and treated in the private sector.” Globally, India tops the list of countries with a high incidence of TB — 56% of estimated cases in 2016 were, in descending order, from India, Indonesia, China, the Philippines and Pakistan, according to the Global TB Report 2017.
- In MDR/RR TB, India, along China and the Russian Federation, accounted for 47% of the global incidence. MDR TB is the most basic form of drug-resistant TB, defined as an infection that does not respond to isoniazid and rifampicin, the two most powerful anti-TB drugs. RR TB is resistant only to rifampicin.
How are consistently high TB numbers to be reconciled with claims of success in the fight against the disease?
- The increase in cases is actually one of the better bits of news on the TB front; this is because it is indicative not of an increased incidence, but of better reporting of the disease.
- In 2012, the government made it mandatory to report all TB cases — the intention was to ensure that patients treated in the private sector, who frequently drop out before completing the full course of antibiotics, leading to drug-resistant forms of the TB bacteria, remain on the government radar, and there is some mechanism to reduce the dropout rates.
- This has led to the increase in TB notifications — in fact, a senior Health Ministry official recently said at an informal interaction that the Ministry was worried “that the number of cases isn’t rising fast enough”.
- What the official meant was that a large number of TB patients could still be lying below the radar, continuing to spread the disease while not being fully cured of it. The WHO Report, too, flagged this: “Ten countries account for 76% of the total estimated gap between TB incidence and notifications, with India, Indonesia and Nigeria accounting for almost half of the total.”
What is the government doing to reach patients who have gone off the radar?
- The government has launched a web-based application called Nikshay to enable health functionaries at various levels across the country to monitor TB cases in their areas.
- Patients receive daily SMSes to ensure they continue their medication. The medicines come with a toll free number that is visible only after the medicine has been taken out of the foil pack; patients are required to give the number a missed call.
- Every missed call is tracked, and when there are too many gaps, the patient is traced, often by treatment supervisors who travel to remote areas on bikes that the programme pays for.
- The TB elimination plan also has incentives for patients and private practitioners.
How does the TB bacteria become resistant to some drugs?
- Typically this happens when the patient does not complete the full course of medication. Depending on the drug and severity of the infection, TB medication may have to be taken for up to 9 months. If a patient drops out along the way, the bacteria is exposed to the drug, but is not killed.
- The organism in this case often mutates in such a way that the drug no longer remains effective.
- This patient, whose symptoms may be in remission (the reason why he or she stopped taking the medication), remains capable of infecting others with the mutated bacteria, and new patients who catch the disease will report drug resistance.
Source:Indian Express
